All about prescription drug coverage

How do I know if my pharmacy is in-network?
Most major pharmacies are in-network. There's no coverage for out-of-network (OON) pharmacies, so you might have to cover the full cost of your meds and vaccinations if you go that route. If you do end up at an OON pharmacy, here are a few tips:
- Ask the pharmacist for a couple of days of medication until you can find an in-network pharmacy
- Search for medication in the app. If it doesn’t appear there, call the pharmacy number on your Surest member ID card for more information
How do I find pharmacy information?
Search for medication directly in the Surest app, or check the pharmacy information on your Surest member ID card. Call Member Services with cost or coverage questions.
Remember: Shopping around is part of the intuitive Surest plan design. When you can check prices in advance and compare options, you may find opportunities to save.
Your pharmacy benefit is managed differently than your medical benefit. For Surest members, that means your Pharmacy Benefit Manager (PBM) is either Navitus or Optum Rx. As such, some benefits may be dually covered by pharmacy and medical. This is especially true for durable medical equipment (DME). Compare prices and coverage.
What is prior authorization? What do I need to do?
Prior authorization (PA) is basically a check to make sure the medication you need is really necessary and covered by your plan. If you’re using in-network providers, they'll handle the prior authorization for you. But if you're seeing someone out of network, you'll need to get that authorization sorted out before your appointment. You can find the Surest prior authorization list online. To see if your medication needs prior authorization, get the procedure codes from your provider, or call 877-237-0006. It’s a good idea to ask your out-of-network provider if they can handle the prior authorization for you. It's usually more efficient if they do it on your behalf.
What’s step therapy?
Step therapy protocol is a common, cost-control strategy where a plan requires you to try one or more less expensive, but often similarly effective, medications before “stepping up” to a more expensive option. Read this guide to learn more about step therapy exceptions.
What’s a formulary?
Also known as a drug list, this is a list of prescription drug medications your Surest health plan covers.
Other helpful tips when looking up a prescription:
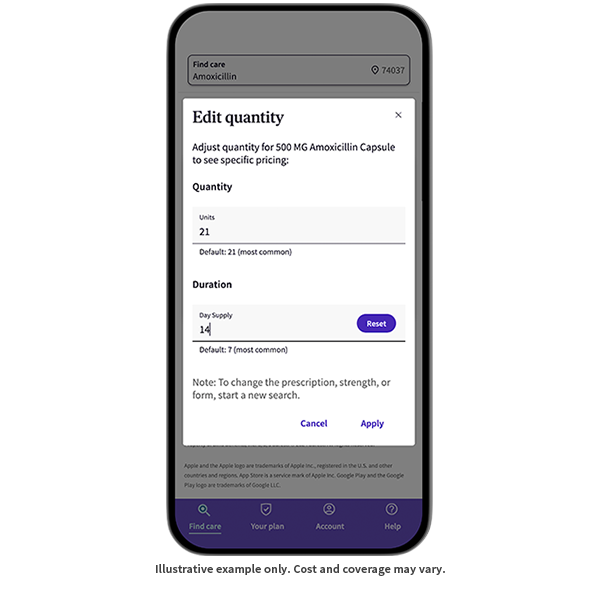
Quantity
Did you know you can control units and duration (supply) in the “quantity” selector of search? (By default, the quantity and duration will set to the most commonly dispensed amounts.)
You’ll see if a brand is a specialty drug, is not covered, is not covered without an alternative, or is not covered but has a covered alternative. You’ll also see if it includes:
- Prior authorization
- Step therapy
- Plan limits
Need to tweak your Rx quantity? Just use the information pop-up/tooltip modal to return to the care options page, or simply navigate back.
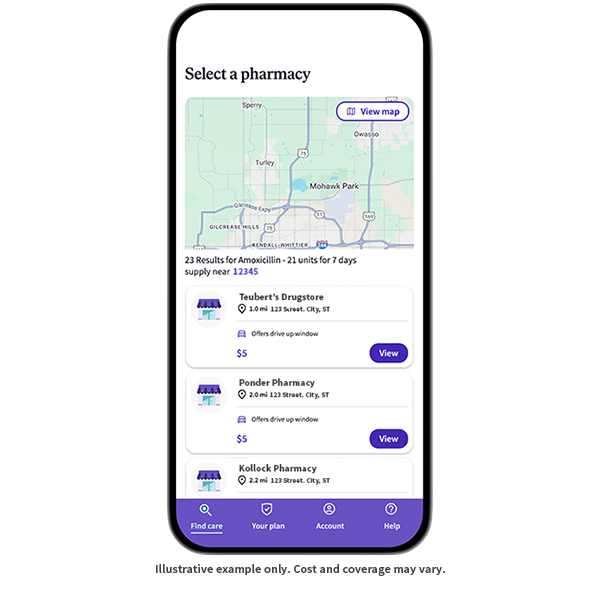
Select a pharmacy
A maximum of 10 pharmacy locations will populate. If multiple locations of the same pharmacy pop up, identical prices will be listed.
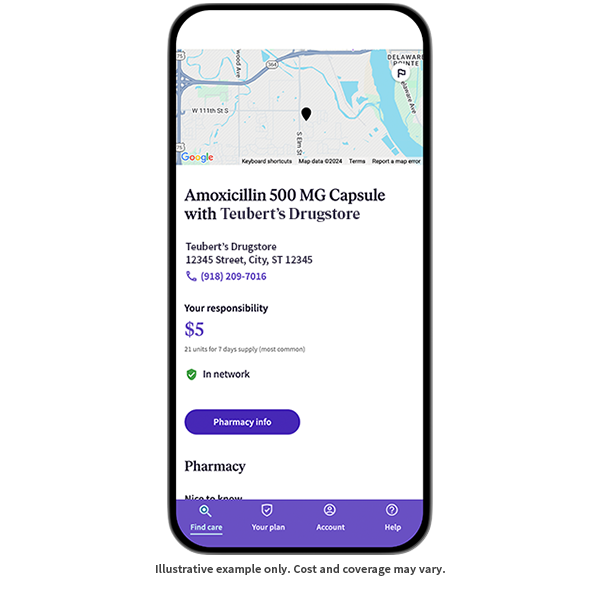
Get more details
When you select a pharmacy, you’ll see contact info, hours of operation, and—in the “Nice to know” section—additional details like drive-up and delivery options.
Was this helpful?
© 2016 - 2024 Healthwise, Incorporated. This information does not replace the advice of a doctor.
This content is not medical advice. You should always consult with your health care professional.